Course Content
-
Pediatric Heart Failure: “How to approach the management of Pediatric Heart Failure” Understanding heart failure: the basics in pediatric heart failure and congenital heart diseases. Basics of treatment and decision making in clinic cases
- Introduction. Definition of Heart Failure
- Etiology of Heart Failure in pediatric age
- Pathophysiology of Heart Failure
- Heart Failure in Congenital Heart Disease
- Natriuretic peptid system
- Biomarkers in Heart Failure
- Signs and Symptoms in pediatric age
- Classification of severity in pediatric Heart Failure
- Different forms of cardiomyopathies: “Diagnostic techniques and treatments”
- Dilated Cardiomyopathy
- Myocarditis
- Hypertrophic Cardiomyopathy
- Restrictive Cardiomyopathy
- Non-compaction Cardiomyopathy
- Arrhythmogenic Right Ventricular Dysplasia (ARVD)
- Evaluation Cardiomyopathies and Genetics
- Evaluation Quiz
- Arrhythmias in Pediatric Heart Failure: EKG abnormalities
- Indications ICD in adults and pediatric age
- Clinic Cases. Quiz
- Treatment in chronic pediatric Heart Failure
- New treatment: Sacubitril – Valsartan
- New therapies and Experimental
- Summary Pediatric Heart Failure therapies
-
Basic and Advanced Echocardiography in Pediatric Heart Failure Description of basic and advanced echocardiography tools for diagnostic and follow-up of children affected by heart failure
- Journal Club: “Basic and advanced echocardiography in advanced heart failure: an overview”
- LV systolic function
- RV systolic function
- Cardiac Diastolic Function and Diastolic Heart Failure
- Tissue Doppler Imaging (DTI) and diastolic dysfunction
- Summary Echo left diastolic dysfunction
- RV diastolic dysfunction
- Management of pediatric diastolic dysfunction
- Clinic Cases
- dP/dt LV function assessment
- Myocardial Performance Index (Tei Index) Doppler Mitral Flow
- Myocardial Performance Index (Tei Index) DTI
- Basics of Strain and Strain-rate
- Global longitudinal Strain (GLS)
- Cardiac output assessment by Echo
- Advanced Imaging in Pediatric Heart Failure
- Echocardiography: Apps and webs
- Clinic Cases
-
Pediatric Heart Transplant (I) Basic in inmunology and rejection. Indications of pediatric heart transplant and contraindications. Mechanical support in pediatric age. Surgery and perioperative treatment.
- Basis of transplant immunology
- Human leucocytes antigen (HLA)
- Blood group antigen (ABO)
- Graft Rejection
- Donor selection & evaluation
- Tissue typing and cross matching
- Ischemic time and the TransMedics® Organ Care System (OCS™)
- Indications and Contraindications of Pediatric Heart Transplant
- Indications of pediatric Mechanical cardiac support (MCS)
- Types of Devices for pediatric MCS
- VAD selection for pediatric MCS
- Surgery of Heart Transplant in pediatric age and in Congenital heart disease
- Principle Challenge in immunosuppressive therapies
- Induction therapy during surgery, postoperative period and denervated heart
-
Pediatric Heart Transplant (II) Basic of immunosuppression treatment. Management of rejection and infections in pediatric heart transplant. Information for patients and relatives. Outcomes of heart transplant and indications of retransplantation
- Basis of immunosuppression therapy
- Risk of infection after transplantation
- Complication of chronic immunosuppression
- Basis of Rejection and assessment
- Endomyocardial biopsy and rejection
- Treatment of humoral and cellular rejection
- Chronic rejection: Coronary Artery Vasculopathy (CAV)
- Clinic follow-up in patient transplanted
- Cardiac Rehabilitation in pediatric heart transplant
- Survival and Causes of death in pediatric heart transplant
- Indications of retransplantation and survival
- Home Care after Pediatric Heart Transplant
- Palliative care in Pediatric Heart Failure and Heart Transplantation
- Future perspectives. Summary
- Clinic cases
-
Final Quizz Congratulations! You finished the course, check your knowledge with this final test
-
Fellow Evaluation Course Evaluation of the cardiac fellows who attended the course in May 2020
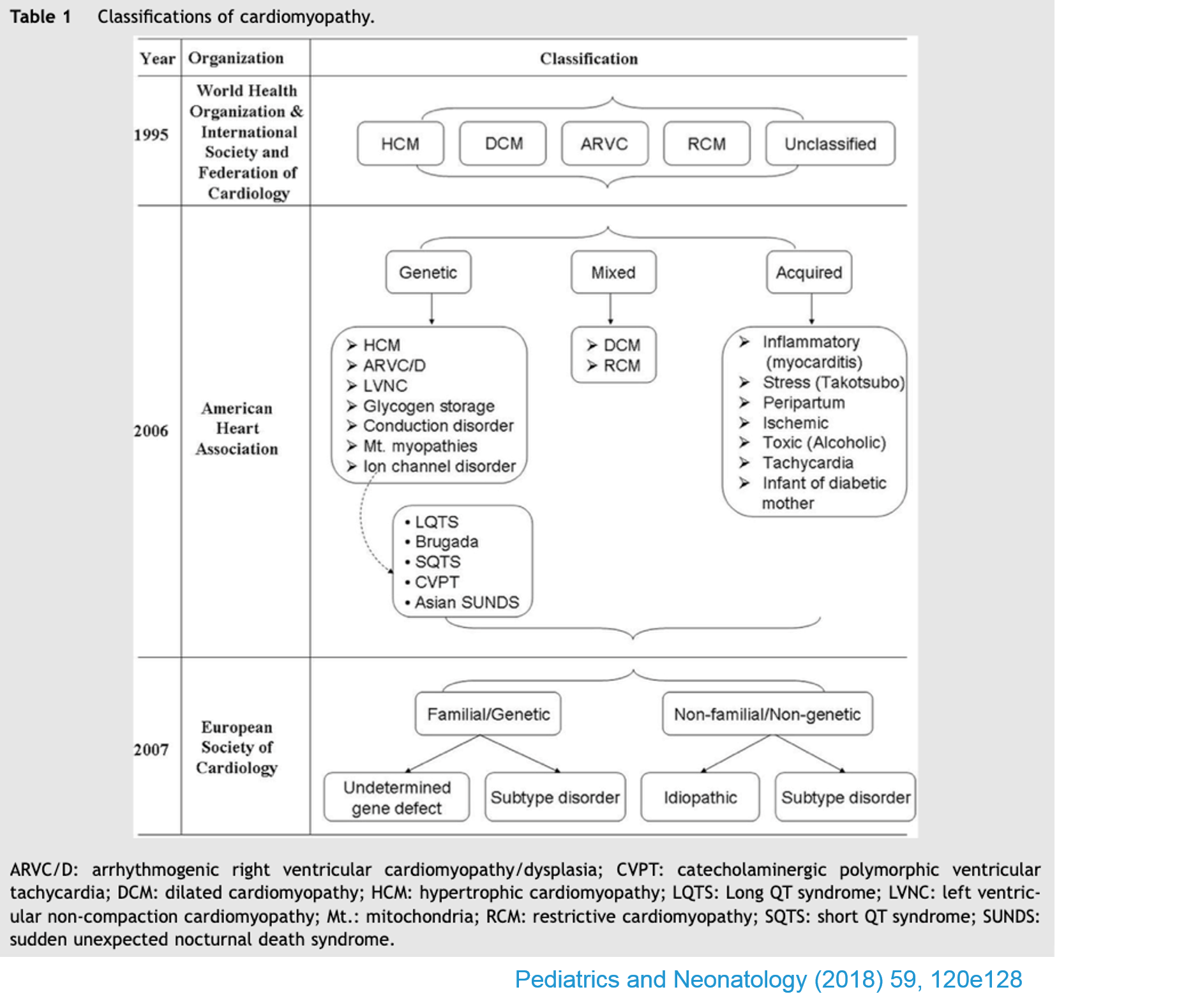
Different forms of cardiomyopathies: “Diagnostic techniques and treatments”
Please, review article of Pediatric cardiomyopathies previous to next lessons.
- Primary Cardiomyopathies: Disease of myocardium in which heart muscle is structurally and functionally abnormal in the absence of coronary disease or abnormal loading conditions (Valvar/CHD/Hypertension etc). Cardiomyopathies were defined as primary myocardial disorders of unknown cause; heart muscle disorders of known aetiology or associated with systemic disorders were classified as secondary or specific heart muscle diseases. Pediatric cardiomyopathies can result from coronary artery abnormalities, tachyarrhythmias, exposure to infection or toxins, or secondary to other underlying disorders.
- The incidence of primary CM in developed countries is reported to be between 0.8 and 1.3 cases per 100,000 children. Account for 60% of children requiring a cardiac transplant
- Because the accuracy and availability of genetic testing has increased, the importance of genetic mutations in the development of pediatric cardiomyopathies has become apparent. Pediatric cardiomyopathies are genetically heterogeneous with many different causative genes and multiple mutations in each gene. Variants in the same gene can cause different phenotypes.
Echocardiography establishes the cardiac phenotype and is performed serially during follow-up and helps to determine prognosis and changes in the treatment. In addition to clinically assessing for heart failure, evaluating the child with cardiomyopathy includes searching for an underlying metabolic, congenital, or acquired cause. This is particularly important in the infant population, where the incidence of metabolic disease is greater and includes potentially reversible conditions, such as primary carnitine deficiency.
Mutations in genes encoding components of the sarcomere or costamere and related binding proteins, Z-band, nuclear membrane, desmosome, mitochondrial, and calcium-handling proteins have all been found in children with cardiomyopathy. Pedigree and cardiac study in first degree relatives are recommended.


