Course Content
-
Pediatric Heart Failure: “How to approach the management of Pediatric Heart Failure” Understanding heart failure: the basics in pediatric heart failure and congenital heart diseases. Basics of treatment and decision making in clinic cases
- Introduction. Definition of Heart Failure
- Etiology of Heart Failure in pediatric age
- Pathophysiology of Heart Failure
- Heart Failure in Congenital Heart Disease
- Natriuretic peptid system
- Biomarkers in Heart Failure
- Signs and Symptoms in pediatric age
- Classification of severity in pediatric Heart Failure
- Different forms of cardiomyopathies: “Diagnostic techniques and treatments”
- Dilated Cardiomyopathy
- Myocarditis
- Hypertrophic Cardiomyopathy
- Restrictive Cardiomyopathy
- Non-compaction Cardiomyopathy
- Arrhythmogenic Right Ventricular Dysplasia (ARVD)
- Evaluation Cardiomyopathies and Genetics
- Evaluation Quiz
- Arrhythmias in Pediatric Heart Failure: EKG abnormalities
- Indications ICD in adults and pediatric age
- Clinic Cases. Quiz
- Treatment in chronic pediatric Heart Failure
- New treatment: Sacubitril – Valsartan
- New therapies and Experimental
- Summary Pediatric Heart Failure therapies
-
Basic and Advanced Echocardiography in Pediatric Heart Failure Description of basic and advanced echocardiography tools for diagnostic and follow-up of children affected by heart failure
- Journal Club: “Basic and advanced echocardiography in advanced heart failure: an overview”
- LV systolic function
- RV systolic function
- Cardiac Diastolic Function and Diastolic Heart Failure
- Tissue Doppler Imaging (DTI) and diastolic dysfunction
- Summary Echo left diastolic dysfunction
- RV diastolic dysfunction
- Management of pediatric diastolic dysfunction
- Clinic Cases
- dP/dt LV function assessment
- Myocardial Performance Index (Tei Index) Doppler Mitral Flow
- Myocardial Performance Index (Tei Index) DTI
- Basics of Strain and Strain-rate
- Global longitudinal Strain (GLS)
- Cardiac output assessment by Echo
- Advanced Imaging in Pediatric Heart Failure
- Echocardiography: Apps and webs
- Clinic Cases
-
Pediatric Heart Transplant (I) Basic in inmunology and rejection. Indications of pediatric heart transplant and contraindications. Mechanical support in pediatric age. Surgery and perioperative treatment.
- Basis of transplant immunology
- Human leucocytes antigen (HLA)
- Blood group antigen (ABO)
- Graft Rejection
- Donor selection & evaluation
- Tissue typing and cross matching
- Ischemic time and the TransMedics® Organ Care System (OCS™)
- Indications and Contraindications of Pediatric Heart Transplant
- Indications of pediatric Mechanical cardiac support (MCS)
- Types of Devices for pediatric MCS
- VAD selection for pediatric MCS
- Surgery of Heart Transplant in pediatric age and in Congenital heart disease
- Principle Challenge in immunosuppressive therapies
- Induction therapy during surgery, postoperative period and denervated heart
-
Pediatric Heart Transplant (II) Basic of immunosuppression treatment. Management of rejection and infections in pediatric heart transplant. Information for patients and relatives. Outcomes of heart transplant and indications of retransplantation
- Basis of immunosuppression therapy
- Risk of infection after transplantation
- Complication of chronic immunosuppression
- Basis of Rejection and assessment
- Endomyocardial biopsy and rejection
- Treatment of humoral and cellular rejection
- Chronic rejection: Coronary Artery Vasculopathy (CAV)
- Clinic follow-up in patient transplanted
- Cardiac Rehabilitation in pediatric heart transplant
- Survival and Causes of death in pediatric heart transplant
- Indications of retransplantation and survival
- Home Care after Pediatric Heart Transplant
- Palliative care in Pediatric Heart Failure and Heart Transplantation
- Future perspectives. Summary
- Clinic cases
-
Final Quizz Congratulations! You finished the course, check your knowledge with this final test
-
Fellow Evaluation Course Evaluation of the cardiac fellows who attended the course in May 2020
Induction therapy during surgery, postoperative period and denervated heart
Post-operative management in CSICU
- Milrinone infusion at a dose of 0.5 mcg/kg/min.
- Isoproterenol infusion for the first 72 hours at starting dose of 0.05 mcg/kg/min can be used in selective cases with low HR and not possible atrial pacing.
- Nitric oxide 20 ppm started in the operating room prior to discontinuation of cardiopulmonary bypass for patients with known or suspected pulmonary hypertension.
- Adequate sedation during the first 24 hours with attention to bleeding, comfort, safety, and adequate cardiopulmonary support.
- Adequate ventilator support with the arterial pO2 > 80 mmHg and the arterial pCO2 < 35 mmHg with goal of arterial pH > 7.40 in the early post-operative period.
- Early identification of right-sided failure and low cardiac output post-transplant secondary to pulmonary hypertension or other issues with surgery and/or graft function. The heart transplant recipient should be considered early for ECMO to allow rest and recovery during the vulnerable peri-operative period. The transplant surgeon and cardiologist should be notified immediately of concerns for graft dysfunction.
- Maintenance immunosuppression (see Table below corresponding to KFSH&RC protocol)
- Treatment of infection and phrophylaxis anti CMV (duration depending status donor-recipient), fungus and Pneumocystis.
- First Endomyocardial Biopsy should be done at 10 days – 2 weeks after transplant (except in children < 1 year of age)
Post-operative assessment in CSICU
- Clinical – vital signs; fever, tachycardia, hypotension or shock– features of hyperacute rejection
- Investigations: Crossmatch results normally at 24 hr. after transplant (if positive risk of humoral rejection), ECHO in OR (TEE) and first days should be done to check biventricular function and data of rejection, Endomyocardial Biopsy at 10 days to check data of rejection (mononuclear infiltrates, fibrinoid necrosis, interstitial hemorrhage. etc), markers of infection and cultures to rule out infection and CMV PCR status each week.
Denervated heart post-transplant
During the surgey of heart transplant, the cardiac plexus is interrupted, and the heart is partially denervated. First days the heart rate and electrical activity of the new heart are purely dependent on the intrinsic electrical system of the heart, not on the neurologic input from the recipient. The resting heart rate is usually higher due to the lack of vagal stimulation which is present at baseline in normal physiology. A higher heart rate is important to augment cardiac output (Cardiac output= Heart rate x Stroke volume), because the donor organ has diastolic dysfunction initially which adversely effects the stroke volume. Isoproterenol, or pacing, can be used to support heart rate. Although cardiac denervation occurs immediately after HTx, cardiac reinnervation is a variable phenomenon and could normalize after days or weeks post-transplant.
INDUCTION AND IMMUNOSUPPRESSION FIRST POSTOPERATIVE DAYS: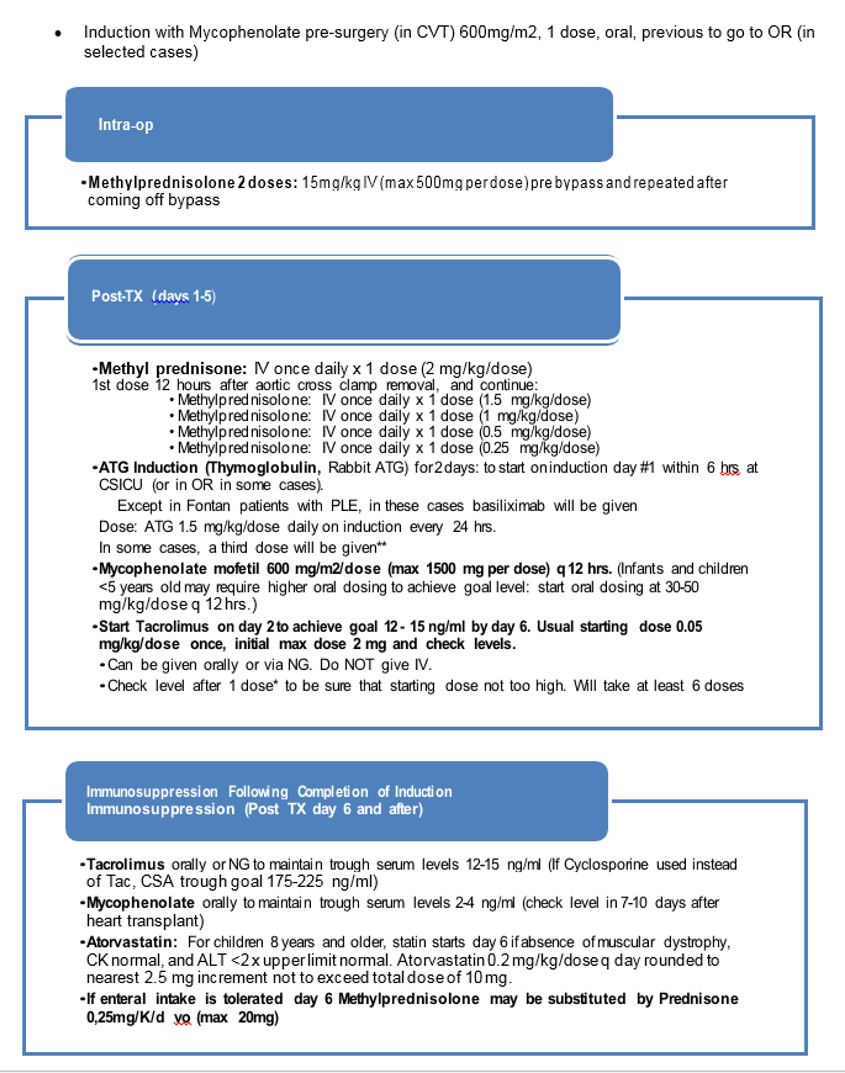
Thymoglobulin® is recommended for heart transplant patients based on the best available evidence: Zuckermann AO, et al. Improved long-term results with thymoglobulin induction therapy after cardiac transplantation: a comparison of two different rabbit-antithymocyte globulines. Transplantation. 2000 May 15;69(9):1890-8.


