Course Content
-
Pediatric Heart Failure: “How to approach the management of Pediatric Heart Failure” Understanding heart failure: the basics in pediatric heart failure and congenital heart diseases. Basics of treatment and decision making in clinic cases
- Introduction. Definition of Heart Failure
- Etiology of Heart Failure in pediatric age
- Pathophysiology of Heart Failure
- Heart Failure in Congenital Heart Disease
- Natriuretic peptid system
- Biomarkers in Heart Failure
- Signs and Symptoms in pediatric age
- Classification of severity in pediatric Heart Failure
- Different forms of cardiomyopathies: “Diagnostic techniques and treatments”
- Dilated Cardiomyopathy
- Myocarditis
- Hypertrophic Cardiomyopathy
- Restrictive Cardiomyopathy
- Non-compaction Cardiomyopathy
- Arrhythmogenic Right Ventricular Dysplasia (ARVD)
- Evaluation Cardiomyopathies and Genetics
- Evaluation Quiz
- Arrhythmias in Pediatric Heart Failure: EKG abnormalities
- Indications ICD in adults and pediatric age
- Clinic Cases. Quiz
- Treatment in chronic pediatric Heart Failure
- New treatment: Sacubitril – Valsartan
- New therapies and Experimental
- Summary Pediatric Heart Failure therapies
-
Basic and Advanced Echocardiography in Pediatric Heart Failure Description of basic and advanced echocardiography tools for diagnostic and follow-up of children affected by heart failure
- Journal Club: “Basic and advanced echocardiography in advanced heart failure: an overview”
- LV systolic function
- RV systolic function
- Cardiac Diastolic Function and Diastolic Heart Failure
- Tissue Doppler Imaging (DTI) and diastolic dysfunction
- Summary Echo left diastolic dysfunction
- RV diastolic dysfunction
- Management of pediatric diastolic dysfunction
- Clinic Cases
- dP/dt LV function assessment
- Myocardial Performance Index (Tei Index) Doppler Mitral Flow
- Myocardial Performance Index (Tei Index) DTI
- Basics of Strain and Strain-rate
- Global longitudinal Strain (GLS)
- Cardiac output assessment by Echo
- Advanced Imaging in Pediatric Heart Failure
- Echocardiography: Apps and webs
- Clinic Cases
-
Pediatric Heart Transplant (I) Basic in inmunology and rejection. Indications of pediatric heart transplant and contraindications. Mechanical support in pediatric age. Surgery and perioperative treatment.
- Basis of transplant immunology
- Human leucocytes antigen (HLA)
- Blood group antigen (ABO)
- Graft Rejection
- Donor selection & evaluation
- Tissue typing and cross matching
- Ischemic time and the TransMedics® Organ Care System (OCS™)
- Indications and Contraindications of Pediatric Heart Transplant
- Indications of pediatric Mechanical cardiac support (MCS)
- Types of Devices for pediatric MCS
- VAD selection for pediatric MCS
- Surgery of Heart Transplant in pediatric age and in Congenital heart disease
- Principle Challenge in immunosuppressive therapies
- Induction therapy during surgery, postoperative period and denervated heart
-
Pediatric Heart Transplant (II) Basic of immunosuppression treatment. Management of rejection and infections in pediatric heart transplant. Information for patients and relatives. Outcomes of heart transplant and indications of retransplantation
- Basis of immunosuppression therapy
- Risk of infection after transplantation
- Complication of chronic immunosuppression
- Basis of Rejection and assessment
- Endomyocardial biopsy and rejection
- Treatment of humoral and cellular rejection
- Chronic rejection: Coronary Artery Vasculopathy (CAV)
- Clinic follow-up in patient transplanted
- Cardiac Rehabilitation in pediatric heart transplant
- Survival and Causes of death in pediatric heart transplant
- Indications of retransplantation and survival
- Home Care after Pediatric Heart Transplant
- Palliative care in Pediatric Heart Failure and Heart Transplantation
- Future perspectives. Summary
- Clinic cases
-
Final Quizz Congratulations! You finished the course, check your knowledge with this final test
-
Fellow Evaluation Course Evaluation of the cardiac fellows who attended the course in May 2020
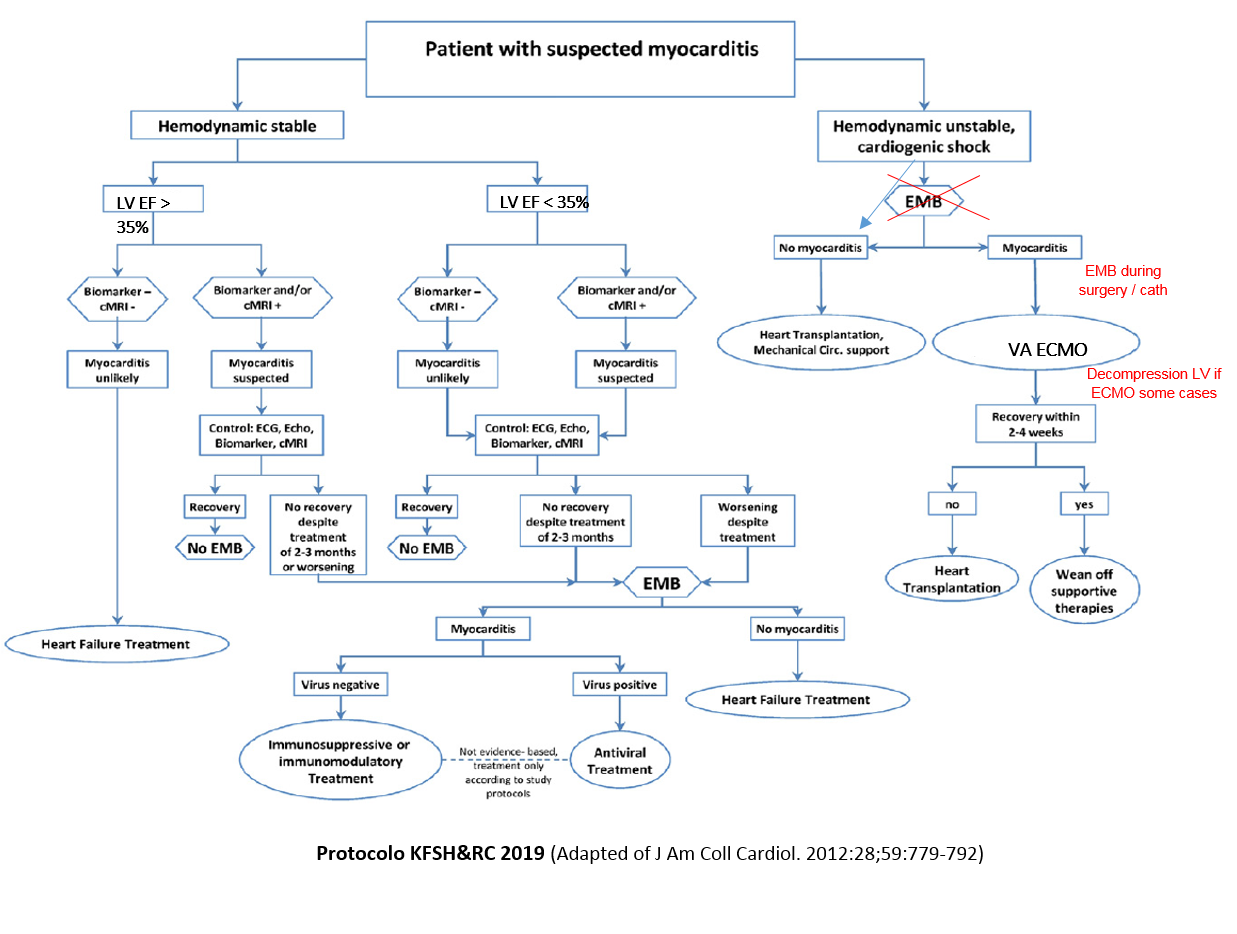
Myocarditis
Acute Myocarditis (AM) is an inflammatory process of the myocardium with associated cardiac dysfunction and up to 30% of the AM patients progress to DCM which is associated with poor prognosis, death or heart transplant. AM should be diagnosed by established histopathological, immunological, and immunohistochemical criteria. It can be associated with any of the following conditions such as viral infections, autoimmune diseases, hypersensitivity/ hypereosinophilic syndromes and sarcoidosis, etc. After excluding all the known causes, a large and more important category of myocarditis is labeled as primary/idiopathic (possibly post viral) myocarditis.
Clinical symptoms may vary from asymptomatic patients to dyspnea, chest pain, heart attack, arrhythmias, or sudden cardiac death. The exact incidence of myocarditis is still not known as an endomyocardial biopsy (EMB) is the gold standard for the histological diagnosis
Pathogenic mechanisms:
AM is often a result of a viral infection that produces myocardial necrosis and triggers an immune response to eliminate the infectious agents (healed myocardium or DCM). Chronic myocardial injury may be caused by post-infectious immune or autoimmune process or develop by a persisting virus infection, responsible for persistent ventricular dysfunction. After a period around 3 months AM produces fibrosis and a permanent myocardium damage.
The sensitivity of cardiac biomarkers, ECG findings and echocardiography are nonspecific. Cardiac MRI could help us to the diagnosis of AM. For proper diagnosis and management of myocarditis, EMB should be performed in patients with acute cardiac deterioration of unknown etiology (more if there is a previous episode of fever) and in patients who are unresponsive to medical therapy. Histological findings have been proved to have prognostic implications (Dallas criteria for inflammation), and in several cases specific treatments can be added (if active virus still remains in myocardium thanks to check PCR virus in myocardium).
Imaging techniques:
-Echocardiography: remains the key method for analyzing ventricular function in AM. Findings are nonspecific, and include global ventricular dysfunction, impaired global longitudinal strain, regional wall motion abnormalities, or diastolic dysfunction.
-Cardiac magnetic resonance (cMRI): can help confirm the diagnosis of myocarditis, especially in the acute phase. Findings of CMR are compatible with myocardial inflammation if at least 2 Lake Louise criteria are met (sensitivity of 76% and specificity of 96%). These include:
- a) Regional or global myocardial signal intensity increase in T2-weighted edema images;
- b) an increased global myocardial early gadolinium enhancement ratio between myocardium and skeletal muscle in gadolinium-enhanced T1-weighted images, and
- c) at least 1 focal lesion with nonischemic regional distribution in inversion recovery-prepared gadolinium-enhanced T1-weighted images.
-EMB. Criteria of Inflammation: The histology of inflammation in the myocardium will be by the qualitative Dallas criteria (presence of inflammatory infiltrates in the myocardium, >_14 leucocytes /mm2, with myocyte degeneration and necrosis of nonischemic cause) and the addition of immunohistochemical criteria > 7.0 CD3+ lymphocytes/mm2 (T cells are CD3 positive).
Treatment:
The basic treatment of myocarditis is the optimal care of heart failure and arrhythmias. Nonconventional and specific treatments depend on the result of the EMB, taking into account the patients’ symptoms and the disease course
–Conventional Treatment of Myocarditis: high doses of IVIg could be used as immunomodulatory effect (just in acute phase). Stable patients with systolic ventricular dysfunction should be treated with diuretics, renin angiotensin aldosterone system inhibitors, and beta-adrenergic blockade (after 1-2 weeks of the acute episode), avoid digoxin in early phases (risks of arrhythmias)
–ECMO support for myocarditis: In patients who develop progressive deterioration of cardiac pump function despite conventional treatment, extracorporeal membrane oxygenation (ECMO) may sometimes be needed as a bridge to recovery, in some cases a decompression LV should be needed
– Specific Treatments: In some patients, inflammation persists due to a post-infectious state or autoimmunity. In case of chronic myocarditis virus-negative patients (confirmed by EMB) the treatment with immunosuppressive agents are indicated (steroids and mycophenolate mofetil-MMF for 6 months):
Steroids: Methyl prednisolone 2mg/kg bolus and 1mg/k/d for 1 month, decreased progressively and doses of maintenance 0,2mg/k/d for 6 months + MMF (Cellcept): 20mg/k/12hr, max 750mg/12hr, levels between 2-4ng/ml: Orders powers as mycophenolic acid)
In case of persistence of virus in cardiac tissue without active inflammation, antiviral treatment will be administered, steroids should be given too if inflammatory data are obtained by EMB. Specific doses and treatments for each of the viruses are summarized in Table. CBC and hepatic profile should be controlled to avoid side effects of interferon during the follow-up.
Summary specific treatment of AM, depending EMB results (children > 1 year)
– Active inflammation + virus: steroids and antiviral treatment
– Active inflammation without virus: steroids and MMF
– Not inflammation + virus: antiviral treatment
– Not inflammation not virus: conventional HF treatment