Course Content
-
Pediatric Heart Failure: “How to approach the management of Pediatric Heart Failure” Understanding heart failure: the basics in pediatric heart failure and congenital heart diseases. Basics of treatment and decision making in clinic cases
- Introduction. Definition of Heart Failure
- Etiology of Heart Failure in pediatric age
- Pathophysiology of Heart Failure
- Heart Failure in Congenital Heart Disease
- Natriuretic peptid system
- Biomarkers in Heart Failure
- Signs and Symptoms in pediatric age
- Classification of severity in pediatric Heart Failure
- Different forms of cardiomyopathies: “Diagnostic techniques and treatments”
- Dilated Cardiomyopathy
- Myocarditis
- Hypertrophic Cardiomyopathy
- Restrictive Cardiomyopathy
- Non-compaction Cardiomyopathy
- Arrhythmogenic Right Ventricular Dysplasia (ARVD)
- Evaluation Cardiomyopathies and Genetics
- Evaluation Quiz
- Arrhythmias in Pediatric Heart Failure: EKG abnormalities
- Indications ICD in adults and pediatric age
- Clinic Cases. Quiz
- Treatment in chronic pediatric Heart Failure
- New treatment: Sacubitril – Valsartan
- New therapies and Experimental
- Summary Pediatric Heart Failure therapies
-
Basic and Advanced Echocardiography in Pediatric Heart Failure Description of basic and advanced echocardiography tools for diagnostic and follow-up of children affected by heart failure
- Journal Club: “Basic and advanced echocardiography in advanced heart failure: an overview”
- LV systolic function
- RV systolic function
- Cardiac Diastolic Function and Diastolic Heart Failure
- Tissue Doppler Imaging (DTI) and diastolic dysfunction
- Summary Echo left diastolic dysfunction
- RV diastolic dysfunction
- Management of pediatric diastolic dysfunction
- Clinic Cases
- dP/dt LV function assessment
- Myocardial Performance Index (Tei Index) Doppler Mitral Flow
- Myocardial Performance Index (Tei Index) DTI
- Basics of Strain and Strain-rate
- Global longitudinal Strain (GLS)
- Cardiac output assessment by Echo
- Advanced Imaging in Pediatric Heart Failure
- Echocardiography: Apps and webs
- Clinic Cases
-
Pediatric Heart Transplant (I) Basic in inmunology and rejection. Indications of pediatric heart transplant and contraindications. Mechanical support in pediatric age. Surgery and perioperative treatment.
- Basis of transplant immunology
- Human leucocytes antigen (HLA)
- Blood group antigen (ABO)
- Graft Rejection
- Donor selection & evaluation
- Tissue typing and cross matching
- Ischemic time and the TransMedics® Organ Care System (OCS™)
- Indications and Contraindications of Pediatric Heart Transplant
- Indications of pediatric Mechanical cardiac support (MCS)
- Types of Devices for pediatric MCS
- VAD selection for pediatric MCS
- Surgery of Heart Transplant in pediatric age and in Congenital heart disease
- Principle Challenge in immunosuppressive therapies
- Induction therapy during surgery, postoperative period and denervated heart
-
Pediatric Heart Transplant (II) Basic of immunosuppression treatment. Management of rejection and infections in pediatric heart transplant. Information for patients and relatives. Outcomes of heart transplant and indications of retransplantation
- Basis of immunosuppression therapy
- Risk of infection after transplantation
- Complication of chronic immunosuppression
- Basis of Rejection and assessment
- Endomyocardial biopsy and rejection
- Treatment of humoral and cellular rejection
- Chronic rejection: Coronary Artery Vasculopathy (CAV)
- Clinic follow-up in patient transplanted
- Cardiac Rehabilitation in pediatric heart transplant
- Survival and Causes of death in pediatric heart transplant
- Indications of retransplantation and survival
- Home Care after Pediatric Heart Transplant
- Palliative care in Pediatric Heart Failure and Heart Transplantation
- Future perspectives. Summary
- Clinic cases
-
Final Quizz Congratulations! You finished the course, check your knowledge with this final test
-
Fellow Evaluation Course Evaluation of the cardiac fellows who attended the course in May 2020
Surgery of Heart Transplant in pediatric age and in Congenital heart disease
Operative method of transplantation in neonates and young infants with cardiomyopathy is the same as for adults with the option of utilizing profound hypothermic circulatory arrest. Method of transplantation in neonates and young infants with hypoplastic left heart syndrome is somewhat different because the portion of donor aorta distal to the arch vessels has to be anastomosed to the neoaorta in the recipient. In some cases, a heart lung transplant has to be performed and surgery differs.
Orthotopic Heart Transplant: Bicaval technique
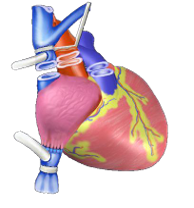 In children with cardiomyopathy, the operative method of transplantation is the same as it is in adults. A median sternotomy is made, a thymectomy is performed, and the recipient’s native heart is exposed. If the donor heart is significantly larger than the native heart, the entire left pericardium anterior to the phrenic nerve is removed. A standard orthotopic technique using bicaval connection is used.
In children with cardiomyopathy, the operative method of transplantation is the same as it is in adults. A median sternotomy is made, a thymectomy is performed, and the recipient’s native heart is exposed. If the donor heart is significantly larger than the native heart, the entire left pericardium anterior to the phrenic nerve is removed. A standard orthotopic technique using bicaval connection is used.
In general, bicaval anastomosis is the best technique used to minimize sinus node dysfunction and to maintain optimal tricuspid annulus configuration. Patients <10 kg at transplant could be underwent biatrial anastamosis to minimize vena caval stenosis.
During the cardiac transplantation procedure, the ventricles are excised, leaving the great vessels, right atrium, and left atrium of the recipient. The donor heart is then sewn to these areas.
Complex cardiac anomalies in heart transplant
Although intracardiac congenital malformations are replaced during heart transplant, extracardiac malformations (congenital, acquired, or iatrogenic) can present considerable challenges to the operative team. Before transplantation, a full comprehension of the operative plan for the management of each individual patient is essential for both the donor team and the recipient surgical
In some cases, some techniques have to be done to adapt the different variants of anatomic anomalies existing between the recipient and donors. The most common congenital abnormalities that require reconstruction at the time of heart transplant are: left superior SVC, absence of IVC, management of position of the great arteries, primary reconstruction of pulmonary arteries following prior congenital procedures or comprehensive reconstruction after prior hybrid type palliation (Chen J. Heart Transplant: Transplantation for Congenital Heart Disease, 2014).
Biventricular, complex congenital heart anomalies, such as transposition of the great arteries, can often be managed by means of direct anastomosis if sufficient lengths of donor arterial and venous connections are procured.


